There’s a moment that catches most families off guard. Maybe it’s a parent recovering from hip surgery, a spouse managing a chronic illness, or a grandparent who simply can’t move around the house like they used to.
Suddenly, you’re Googling things like “home nursing care” at 2 AM, trying to figure out what’s available, what it costs, and whether it’s actually worth it.
Here the thing home nursing care and medical healthcare services have changed dramatically over the past decade. What used to require a hospital stay can now happen in your living room. The options are far more varied (and more affordable) than most people realize.
This guide breaks down everything you need to know from the types of care available to how insurance works, what to look for in a provider, and the questions you should ask before signing anything.
What Exactly Is Home Nursing Care?
Home nursing care is professional medical assistance delivered in a patient’s home rather than in a hospital or clinic. It sounds simple, but the scope is surprisingly broad.
A registered nurse might visit three times a week for wound care after surgery. A licensed practical nurse could stop by daily for insulin injections. A home health aide might help with bathing, dressing, and meals.
The key distinction to understand is skilled nursing care vs. non-medical home care:
- Skilled nursing care involves clinical tasks like IV therapy, catheter management, medication adjustments, and vital sign monitoring
- Non-medical home care covers personal assistance like grooming, light housekeeping, companionship, and transportation to appointments
Types of Medical Healthcare Services Available at Home
The range of medical healthcare services available at home today would have seemed impossible twenty years ago. Here’s what’s out there.
Skilled Nursing Services:
Registered nurses and licensed practical nurses handle a wide variety of clinical tasks at home, including:
- Post-surgical wound care
- Injections and infusions
- Pain management
- Chronic disease monitoring (diabetes, heart failure)
- Ventilator care
- Patient and family education
Skilled nurses also teach patients and families how to manage conditions between visits, which makes a real difference in long-term outcomes.
Physical, Occupational, and Speech Therapy:
Rehabilitation doesn’t have to happen in a clinic. Licensed therapists come to the patient’s home to work on mobility, strength, balance, daily living skills, and communication.
Home-based therapy has a distinct advantage therapists can tailor exercises to the exact environment where the patient lives. They teach patients how to navigate their own stairs, kitchen, and bathroom safely.
Palliative and Hospice Care:
For patients dealing with serious illness, palliative care focuses on comfort and quality of life without necessarily stopping curative treatment. Hospice care is specifically for end-of-life situations.
Both can be delivered at home with a team that typically includes:
- Nurses
- Social workers
- Chaplains
- Trained volunteers
Families consistently report that receiving this kind of care at home brings more peace and dignity to a difficult time.
Chronic Disease Management Programs:
Many home healthcare agencies now offer structured programs for conditions like congestive heart failure, COPD, and diabetes.
These programs involve regular nurse visits, remote monitoring through wearable devices, medication management, and coordinated communication with the patient’s physician. The goal is simple — keep people stable and out of the emergency room.
Telehealth and Remote Patient Monitoring:
This is one of the fastest-growing areas in home health care. Patients use connected devices that send data directly to their care team:
- Blood pressure cuffs
- Glucose monitors
- Pulse oximeters
- Smart scales
- Fall detection sensors
A nurse or physician reviews the numbers and can step in early if something looks off. It’s not a replacement for in-person care, but it fills the gaps between visits brilliantly.
Medical Social Work Services:
Here’s a service most people don’t think about, but it’s incredibly valuable.
Medical social workers visit the home and help patients and families navigate the emotional, financial, and logistical side of dealing with illness. They connect you with community resources, assist with advance directive planning, help resolve insurance issues, and provide counseling during tough transitions.
If your family feels overwhelmed by the “everything else” that comes with a health crisis — not just the medical part — a social worker can take a huge weight off your shoulders.
Dementia and Alzheimer’s Specialized Care:
For families dealing with memory loss, home-based dementia care deserves its own mention.
Trained caregivers use specific communication techniques, structured daily routines, and safety supervision designed for patients with cognitive decline. Keeping someone with Alzheimer’s in a familiar environment reduces confusion and agitation significantly compared to an unfamiliar facility.
Many agencies now employ caregivers with specialized dementia training who understand how to redirect behaviors, maintain dignity, and create calm, predictable routines.
Home-Based Laboratory Testing and Nutritional Support:
Something many families don’t realize is that basic lab work can be done right at home:
- Blood draws
- Urine tests
- Portable X-rays
This eliminates stressful trips for patients with mobility issues or weakened immune systems.
Registered dietitians can also visit the home to assess nutritional needs, create meal plans for specific conditions (kidney disease, diabetes), and train caregivers on proper food preparation. For patients who can’t cook, many communities offer Meals-on-Wheels programs delivering hot meals several times a week.
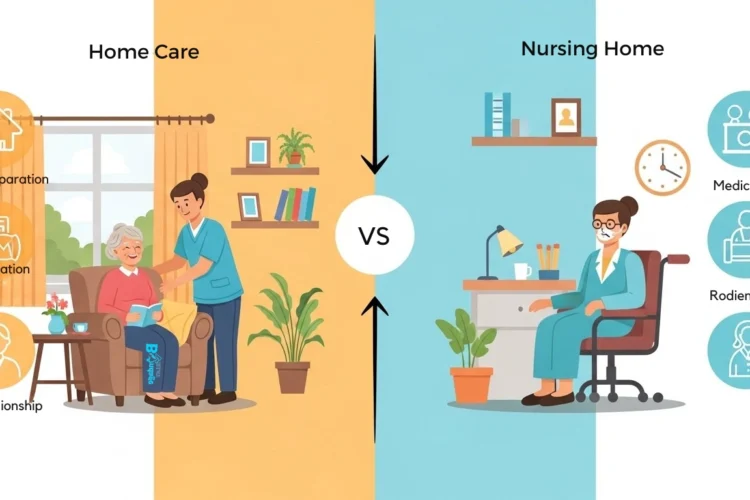
| Factor | Home Nursing Care | Hospital / Nursing Facility |
| Environment | Familiar home setting | Clinical, institutional setting |
| Cost (average per day) | $150 – $350 | $800 – $2,500+ |
| Infection Risk | Lower exposure to hospital-acquired infections | Higher due to shared spaces and equipment |
| Personalization | One-on-one, highly individualized | Shared attention among multiple patients |
| Family Involvement | High — family stays actively involved | Limited by visiting hours and policies |
| Recovery Speed | Often faster due to comfort and reduced stress | Can be slower due to disrupted routines |
| Advanced Equipment | Limited but growing with portable tech | Full access to specialized equipment |
| Emotional Well-Being | Patients feel more independent | Can cause feelings of isolation and anxiety |
| Insurance Coverage | Medicare, Medicaid, and most private plans | Covered, but co-pays are often higher |
Who Actually Benefits from Home Nursing Care?
It’s tempting to think of home healthcare as something only elderly people need. The reality is much broader.
Seniors with Chronic Conditions:
This is the largest group. Older adults managing heart disease, diabetes, arthritis, or dementia benefit enormously from consistent in-home monitoring.
Regular nurse visits catch problems early. A slight change in weight might signal fluid retention in a heart failure patient, for instance before it snowballs into a hospital admission.
Post-Surgical Patients:
Anyone recovering from major surgery (joint replacement, cardiac surgery, abdominal procedures) often does better at home once they’re medically stable.
Home nurses manage wound care, monitor for complications, and coordinate physical therapy. Patients sleep better, eat better, and generally heal faster in their own beds.
Children with Complex Medical Needs:
Pediatric home nursing is a lifeline for families with children who have conditions like:
- Cerebral palsy
- Genetic disorders
- Technology dependence (feeding tubes, ventilators)
Having skilled nurses at home allows these children to grow up in a family environment rather than a medical facility. That has profound effects on their development and quality of life.
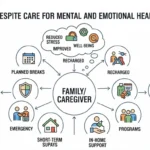
Adults Managing Mental Health Conditions:
Some home healthcare programs now include psychiatric nursing visits for patients dealing with severe depression, bipolar disorder, schizophrenia, or anxiety disorders.
These nurses help with medication compliance, symptom monitoring, and connecting patients to community resources. It’s a growing area that fills a real gap in mental health care access.
How to Choose the Right Home Healthcare Provider
Not all home nursing agencies are created equal. Picking the wrong one can create more stress than it relieves. Here’s what actually matters.
Verify Licensing and Accreditation:
Every legitimate agency should be licensed by your state’s health department. Beyond that, look for accreditation from The Joint Commission or the Community Health Accreditation Partner (CHAP).
Accreditation isn’t legally required, but agencies that pursue it voluntarily are signaling they take quality seriously.
Ask About Staff Qualifications and Training:
Find out what kind of background checks the agency runs. Ask about hiring standards — do they require minimum years of experience? What about ongoing training?
The best agencies invest in continuing education and have clear protocols for handling emergencies.
Understand the Care Plan Process:
A reputable provider conducts a thorough initial assessment before care begins. This should include:
- A registered nurse visiting the home
- Evaluating the patient’s needs and medical history
- Assessing the home environment for safety concerns
- Creating a detailed care plan with the patient’s physician
If an agency wants to start sending people over without this step, that’s a red flag.
Check Reviews and References:
Online reviews tell part of the story, but not the whole picture. Ask the agency for references — specifically, families who had similar care needs to yours.
You can also check Medicare’s Home Health Compare tool, which rates agencies based on quality measures, patient satisfaction, and hospital readmission rates.
Evaluate Communication Practices:
How does the agency communicate with families? Do they provide regular updates? Is there a care coordinator you can reach with questions?
Smooth communication isn’t a luxury it’s what prevents mistakes and keeps everyone on the same page.
Understanding Insurance Coverage for Home Healthcare
Insurance is where things get complicated, but understanding the basics can save you thousands of dollars.
Medicare Coverage:
Medicare covers home health services if the patient meets these criteria:
- They must be homebound (leaving home requires considerable effort)
- They need skilled nursing care or therapy
- A doctor certifies that home healthcare is medically necessary
When these conditions are met, Medicare pays 100% with no co-pay or deductible. That surprises a lot of people.
However, Medicare does not cover:
- 24-hour-a-day care at home
- Custodial care (daily activity help when that’s the only need)
- Meal delivery
- Homemaker services when no skilled need exists
Understanding these limits upfront prevents painful surprises later.
Medicaid Coverage:
Medicaid covers home healthcare in every state, but specifics vary widely.
Many states offer Home and Community-Based Services (HCBS) waivers that cover personal care, respite care, and services beyond what Medicare provides. If your family member qualifies for Medicaid, investigate your state’s waiver programs they can be a game-changer.
Private Insurance:
Most private plans cover some form of home healthcare, but details depend on your specific policy. Common requirements include:
- Prior authorization
- A physician’s order
- Demonstrated medical necessity
Review your policy carefully or call your insurer to ask specifically about home health benefits, visit limits, and out-of-pocket costs.
Veterans Affairs (VA) Home Health Benefits:
This is one of the most underused resources in home healthcare.
Veterans enrolled in the VA healthcare system may qualify for:
- Home-based primary care
- Skilled home nursing
- Homemaker and home health aide services
- Respite care
- Adult day health care
Most of these come at little to no cost. The VA’s Home Based Primary Care (HBPC) program provides comprehensive care right in the veteran’s home for those with complex, chronic conditions.
If your loved one served in the military, contact your local VA medical center. Many families don’t realize these programs exist until years after they could have started using them.
Long-Term Care Insurance:
If you or your loved one purchased a long-term care policy, it likely covers home nursing services.
These policies typically kick in when the insured person can’t perform a certain number of activities of daily living (bathing, dressing, eating) without assistance. Check the policy’s elimination period (waiting time before benefits begin) and daily benefit amount.
The Role of Technology in Modern Home Healthcare
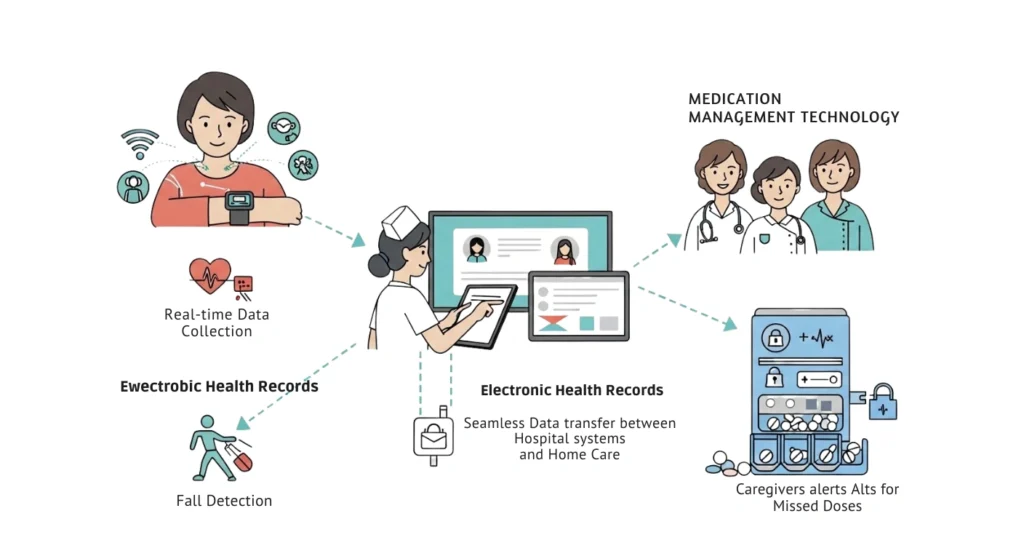
Technology is reshaping what’s possible in home nursing care. These developments are worth paying attention to.
Wearable Health Monitors:
Devices that continuously track heart rate, blood oxygen, blood pressure, and fall detection are becoming standard in home healthcare.
They give care teams real-time data without requiring a nurse around the clock. Some advanced monitors can detect atrial fibrillation or sleep apnea patterns and alert providers automatically.
Electronic Health Records and Care Coordination:
Modern home health agencies use electronic records that sync with hospital systems and physician offices.
Your home nurse can see the same records your doctor sees. When your cardiologist adjusts a medication, your home nurse knows about it the same day. This reduces errors and makes transitions between care settings much smoother.
Medication Management Technology:
Smart pill dispensers are reducing one of the biggest risks in home healthcare medication errors. These devices:
- Alert patients when it’s time to take medication
- Lock to prevent double-dosing
- Notify caregivers of missed doses
- Integrate with pharmacy systems
Combined with pharmacy coordination, these tools make it far safer for patients to manage complex medication regimens at home.
How to Prepare Your Home Before Care Begins
This is something almost nobody talks about. But preparing your home before the first nurse walks through the door makes a massive difference.
Conduct a Home Safety Assessment:
Before home nursing care starts, walk through the house with fresh eyes. Look for:
- Tripping hazards (loose rugs, electrical cords, cluttered floors)
- Stairways without sturdy handrails
- Bathrooms without grab bars near the toilet and shower
- Doorways too narrow for wheelchairs or walkers
Many agencies will send a nurse or occupational therapist for a formal safety assessment, but getting ahead of obvious issues saves time and prevents accidents.
Set Up a Dedicated Care Area:
You don’t need to turn your living room into a hospital ward. But a clean, organized space where the nurse can work makes visits much more efficient.
Set up a well-lit area near an electrical outlet with a comfortable chair or bed, a small table for supplies, and easy bathroom access. Keep all medications, medical records, and insurance documents in one central spot.
Stock Essential Supplies:
Talk to the home health agency before the first visit about what supplies you’ll need. Common items include:
- Disposable gloves
- Wound care supplies
- Thermometer and blood pressure cuff
- Hand sanitizer
- Clean towels
Some items are provided by the agency or covered by insurance, but knowing what to have ready prevents last-minute scrambling.
Prepare for Emergency Situations:
Make sure emergency numbers are posted visibly:
- Home health agency’s after-hours line
- Patient’s physician
- Local emergency services
- Family emergency contact
If the patient has a Do Not Resuscitate (DNR) order or advance directive, keep a copy in an obvious location (like on the refrigerator) so emergency responders can find it immediately. Also make sure the home has working smoke detectors, clear exit paths, and that at least one family member knows basic CPR.
Final Thoughts
Home nursing care and medical healthcare services give families something powerful the ability to receive professional, compassionate medical support without giving up the comfort and dignity of home. Start the conversation early, ask the hard questions, involve your loved one in every decision, and never settle for care that doesn’t feel right.