Nobody dreams of spending their days in a hospital. The fluorescent lights, the constant beeping, the stiff mattresses it all feels worlds away from the comfort of home.
Yet millions of people living with chronic illnesses need ongoing medical care every single day. That’s where home nursing steps in, and honestly, it’s changing the way we think about long-term healthcare.
In the United States alone, over 50% of adults live with at least one chronic condition, and roughly 3 million Americans get care from home health agencies. These aren’t just numbers. They represent real people who want to manage their health at home rather than inside a clinic.
What Exactly Is Home Nursing?
Home nursing means professional healthcare delivered right at a patient’s residence. It goes far beyond basic home help like cooking or cleaning.
Licensed professionals registered nurses, nurse practitioners, and specialized therapists bring hospital-level expertise directly into your living room. Their services typically include:
- Wound care and post-surgical support
- Medication management and administration
- Physical, occupational, and speech therapy
- Vital sign monitoring and health tracking
- Patient and family education
- Care coordination with doctors and specialists
What makes home nursing so appealing is its flexibility. It fits around the patient’s life rather than forcing the patient into a rigid hospital schedule. If you’re managing diabetes, heart disease, COPD, or arthritis, that kind of personalized attention can make a huge difference.
Why Chronic Illness Needs a Different Care Approach
Chronic illnesses don’t work like a broken bone or a bad flu. You can’t just treat them once and move on. They demand ongoing management sometimes for years, sometimes for the rest of your life.
Conditions like diabetes, hypertension, heart failure, and chronic respiratory disease require consistent monitoring, medication adjustments, lifestyle changes, and emotional support.
Here’s the thing traditional hospital care wasn’t built for this. Hospitals handle acute episodes. You go in when something goes wrong, and you leave when the immediate crisis passes.
But what happens in between those visits? That’s where things tend to fall apart. Patients forget medications, miss early warning signs, or just feel overwhelmed trying to manage everything on their own. Home nursing fills that gap with continuous, proactive care delivered right where patients spend most of their time.
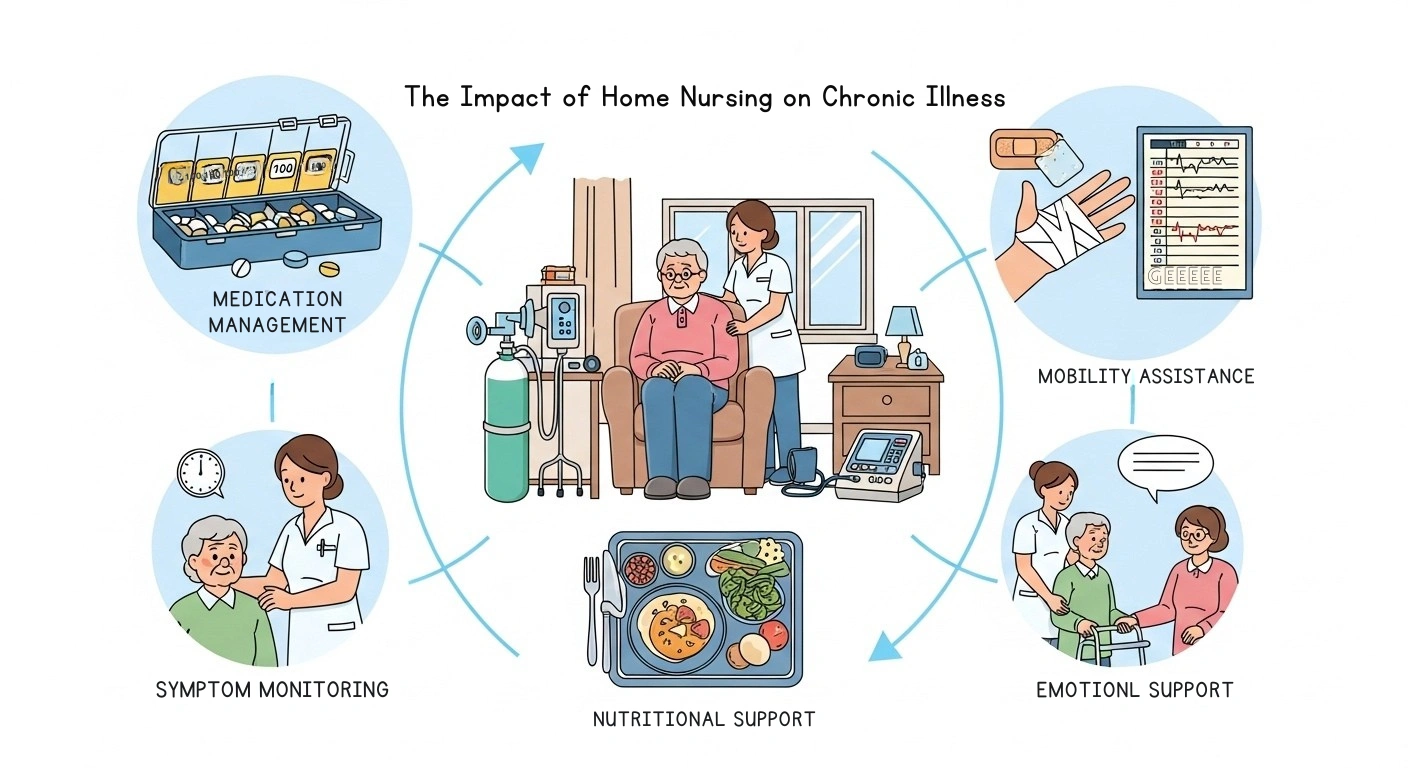
The Medical Benefits of Home Nursing for Chronic Illness
Fewer Hospital Readmissions:
One of the biggest proven advantages of home nursing is that it keeps people out of the hospital. A meta-analysis of 12 randomized controlled trials found that patients who got in home care experienced:
- A 12% drop in risks tied to all-cause mortality and hospitalizations
- One fewer unplanned hospitalization on average
- One fewer emergency department visit compared to conventional care
That’s a win for patients, families, and the entire healthcare system.
Better Medication Management:
If you’ve ever watched someone juggle five or six medications with different dosages and schedules, you know how confusing it gets. Home nurses step in and handle this by:
- Making sure patients take the right medications at the right times
- Watching for side effects and drug interactions
- Preventing accidental double dosing, especially with elderly patients who have memory issues
- Passing medication concerns directly to physicians
Continuous Health Monitoring:
Instead of waiting months for a doctor’s appointment to catch a problem, home nurses track key health numbers on a regular basis, including:
- Blood pressure and heart rate
- Blood sugar levels
- Weight changes and fluid retention
- Oxygen saturation levels
- Wound healing progress
This kind of real-time tracking catches a blood pressure spike or a blood sugar crash before it turns into an emergency room trip.
The Emotional and Psychological Impact
Less Stress and Anxiety:
Living with a chronic illness is already stressful. Add in the hassle of navigating a complicated healthcare system, and it becomes overwhelming. Home nursing takes a lot of that stress away by bringing care directly to the patient.
No arranging transportation. No crowded waiting rooms. No hospital anxiety. Studies show that patients getting long-term home nursing care rate the emotional and informational support from their nurses as one of the most valuable parts of their care.
Keeping Independence and Dignity:
One of the biggest fears people face after a chronic illness diagnosis is losing their independence. Home nursing helps patients hold onto that by allowing them to:
- Stay in their own familiar surroundings
- Keep their daily routines going
- Sleep in their own beds and eat their own food
- Stay close to family, friends, and pets
- Feel in control of their own lives
Research confirms that in-home nursing care helps patients perform daily living activities more easily, with measurable drops in the difficulty they experience doing everyday tasks.
Stronger Family Involvement:
When care happens at home, family members naturally become part of the team. Home nurses don’t just look after the patient they also teach families how to:
- Help with daily care tasks
- Spot warning signs of worsening health
- Offer emotional support without burning out themselves
- Talk effectively with the healthcare team
This teamwork approach builds a stronger support network and helps families feel less helpless during a difficult time.
| Factor | Home Nursing | Hospital or Facility Care |
|---|---|---|
| Environment | Familiar, comfortable home setting | Clinical, institutional environment |
| Personalization | One-on-one, tailored care plans | Standardized protocols for many patients |
| Cost | Generally lower long-term costs | Higher due to facility overhead and staffing |
| Infection Risk | Much lower | Higher risk of hospital-acquired infections |
| Patient Independence | Maintained and encouraged | Often limited by facility routines |
| Family Involvement | High — family takes part in care | Limited by visiting hours and policies |
| Emotional Well-Being | Patients report higher satisfaction | Can lead to anxiety, depression, and isolation |
| Readmission Rates | Lower with consistent home monitoring | Higher without transitional follow-up |
The Financial Side of Home Nursing
Cost Savings for Patients and the System:
Let’s be real chronic illness is expensive. In the United States, over two-thirds of every healthcare dollar goes toward treating chronic conditions. For older adults, that number climbs to nearly 95%.
Home nursing brings those costs down in several important ways:
- No facility overhead or hospital bed to pay for
- Fewer emergency visits when nurses catch problems early
- Lower transportation costs for patients and families
- Reduced infection-related treatment expenses
- One study of over 3,000 Medicare patients showed savings exceeding 30% with targeted home healthcare
The U.S. home healthcare market is growing at about 7.5% annually and will keep expanding through 2030. That growth tells you the system now recognizes home-based care as both effective and affordable.
Insurance and Medicare Coverage:
Medicare covers home health services under certain conditions usually when a patient is homebound and needs skilled nursing care or therapy. Here’s a quick breakdown:
- Days 1 to 20: Medicare covers 100% of skilled nursing facility costs
- Days 21 to 100: Daily copayment of $204 based on recent figures
- After Day 100: Medicare coverage ends, and the patient pays everything
Home nursing can often delay or completely prevent the need for facility-based care, saving patients thousands of dollars. Just make sure you check with your specific insurance provider since coverage details vary quite a bit.
Nutritional Support and Diet Management at Home

Here’s something most healthcare blogs barely mention nutrition. And yet it’s one of the most important parts of managing any chronic illness. A bad diet can undo even the best medication plan.
Home nurses don’t just hand you a pamphlet about healthy eating. They team up with registered dietitians to build personalized meal plans that consider:
- The patient’s specific medical condition
- Current medications and possible food-drug interactions
- Age, cultural background, and personal preferences
- Ability to chew, swallow, and cook independently
What makes home-based nutritional support so powerful is that it happens where the food actually gets made and eaten. A nurse visiting the home can peek inside the fridge, check pantry shelves, and spot real problems that would never come up during a quick clinic visit.
Maybe the patient skips meals because cooking feels exhausting. Or maybe they eat high-sodium canned food because getting fresh groceries is a struggle. These real-world observations let nurses suggest practical fixes rather than generic advice.
For elderly patients, malnutrition is a serious but often invisible risk. Studies show that up to 85% of nursing home residents deal with some form of malnutrition. While the figure is likely lower for people getting care at home, the danger still exists. Home nurses keep an eye on weight, appetite, and eating patterns, catching nutritional decline before it leads to a hospitalization.
Beyond individual meals, nurses also teach family caregivers how to prepare the right foods, read nutrition labels, and notice when a loved one’s eating habits point to a bigger problem. That kind of hands-on, kitchen-table education beats any hospital discharge handout.
How Home Nurses Help Patients Take Charge of Their Health
One of the most overlooked parts of home nursing is patient education. Nurses don’t just give care they teach patients how to care for themselves.
Here’s what that education typically covers:
- Understanding your specific condition and what triggers flare-ups
- Recognizing symptoms that need immediate attention
- Learning about proper nutrition and meal planning
- Building confidence to manage health independently
- Setting realistic and achievable health goals
- Knowing when to call a doctor versus when to handle things at home
This approach turns patients into active partners in their own care rather than people who just sit back and wait for the next appointment.
Research across multiple countries shows that nurses who address the emotional and social sides of chronic illness not just the medical symptoms help their patients enjoy a noticeably better quality of life. Good care isn’t only about treating the disease. It’s about helping someone live well in spite of it.
Disease Acceptance and the Psychology of Living with Chronic Illness
This part doesn’t get talked about nearly enough. When someone finds out they have a chronic illness, medical treatment is only half the battle. The other half is psychological learning to accept and adapt to a life that has permanently changed.
Research from Frontiers in Public Health found a clear link between disease acceptance and quality of life among long-term home nursing patients:
- Patients who accepted their condition reported higher life satisfaction
- They followed treatment plans more consistently
- They experienced less depression and anxiety
- Younger patients struggled with acceptance more than older ones
That makes sense when you think about it. A 35-year-old who just got diagnosed with multiple sclerosis faces a completely different emotional reality than a 70-year-old managing high blood pressure. The younger person may grieve lost career plans, social activities, or physical abilities they assumed would always be there.
Home nurses have a unique advantage here because they see patients in their actual lives — not in a sterile exam room for ten minutes. They notice when someone stops going for walks, loses interest in hobbies, or pulls away from family. Those subtle shifts often signal declining mental health.
Instead of just referring every struggling patient to a therapist, home nurses offer something therapists often can’t consistent, ongoing presence. They build trust over weeks and months. They celebrate small wins like a better blood sugar reading, a short walk around the block, or a full week of sticking to a medication schedule.
Those small moments of encouragement help patients rebuild their sense of control, which sits at the heart of genuine disease acceptance.
Families benefit from understanding this too. Caregivers who recognize their loved one is fighting a psychological battle not just a physical one can respond with empathy instead of frustration. Home nurses often act as a bridge here, coaching family members on how to encourage independence without overlooking real limitations.
The Role of Technology in Modern Home Nursing
Telehealth and Remote Monitoring:
Home nursing has evolved way beyond a nurse with a stethoscope making house calls. Technology now plays a huge role in how care gets delivered:
- Telehealth platforms let nurses and doctors check in through video calls
- Wearable devices track heart rate, blood oxygen, glucose levels, and more in real time
- Electronic health records give every care team member access to the same updated patient information
- The global EHR market should reach over $43 billion by 2034
Smart Devices and Wearables:
Today’s health trackers do much more than count steps. They can:
- Alert nurses to changes in vital signs before the patient even notices
- Track sleep patterns that affect how well someone manages their condition
- Monitor activity levels and flag sudden drops
- Send real-time data to providers for faster decisions
For chronic illness patients, this kind of early detection is incredibly valuable. Small changes caught early can prevent big problems later.
Challenges Home Nursing Still Faces
It wouldn’t be fair to paint a completely rosy picture. Home nursing has real challenges that need honest conversation.
Workforce Shortages:
Demand for home health nurses keeps growing faster than the supply. Registered nurse employment should grow by about 6% through 2032, but the home healthcare sector needs even faster expansion to keep pace with the aging population.
Caregiver Burnout:
Family members who pitch in alongside professional nurses often hit a wall. The emotional and physical toll of caring for a chronically ill loved one at home can be enormous, and affordable respite care isn’t always easy to find.
Uneven Quality:
Not every home nursing agency delivers the same standard of care. Quality depends on the agency, the individual nurses, and local regulations. Families need to research providers carefully before making a choice.
Access Gaps:
People in rural or underserved areas often have trouble getting quality home nursing. Expanding telehealth and remote monitoring tools can help close this gap, but it’s still a work in progress.
Who Benefits Most from Home Nursing?
Home nursing helps a wide range of patients, but some groups see the biggest impact:
- Elderly patients juggling multiple chronic conditions
- People recovering from surgery who need ongoing wound care
- Diabetes patients who require regular blood sugar checks
- Heart failure patients who need daily weight and fluid monitoring
- Those with chronic respiratory diseases who depend on oxygen therapy
- Patients with neurological conditions like Parkinson’s or multiple sclerosis
- Cancer patients receiving ongoing treatment support at home
If you or someone you love fits any of these descriptions, home nursing deserves a serious look.
The Future of Home Nursing for Chronic Illness
The trend is unmistakable home-based care is becoming the backbone of chronic illness management.
With an aging global population expected to hit 2.1 billion people over age 60 by 2050 and chronic disease rates still climbing, hospitals and nursing facilities simply can’t handle everyone. Home nursing offers a patient-centered solution that matches what most people actually want: to live, heal, and manage their health in the comfort of their own homes.
As technology keeps improving and healthcare policies shift toward supporting in-home care, expect home nursing to play an even bigger role in how the world handles chronic illness.
Final Thoughts
The impact of home nursing on chronic illness goes far beyond medical charts and statistics. It shows up in the diabetic grandmother who still tends her garden because a nurse helps with her insulin. It shows up in the heart failure patient who avoids another hospital stay because a routine visit caught a problem early. And it shows up in the family that breathes a little easier knowing a trusted professional walks beside them through the hardest days. Home nursing isn’t perfect and it won’t fit every situation, but for millions living with chronic illness, it offers something truly valuable the chance to heal, manage, and live well, right at home.