Imagine your mom or dad stubbornly insisting they’ll never leave the house they’ve lived in for 50 years. You get it that home holds memories of holidays, kids growing up, and quiet mornings with coffee on the porch. But you also worry. What if they fall when no one’s around, What if a small health scare turns into something bigger because help arrives too late, That’s the reality for millions of families today. Most older adults want to stay right where they are, surrounded by their community, and honestly, who can blame them.
Understand Community-Based Aging
Community-based aging simply means growing older in the place you know and love, staying tied to your neighbors, local shops, and familiar routines. It’s different from moving to a nursing home or assisted living facility. You keep your independence, but you get help when you need it.
Recent numbers show just how much people want this. Surveys from 2025 say about 75% to 84% of adults over 50 plan to stay in their own homes as long as possible. That makes sense your home feels like you. It’s where you’re comfortable. But staying safe takes some planning. That’s where options like live-in care come in, giving you professional support without uprooting your life.
Why Safety Really Matters as We Age
Getting older brings some changes that nobody likes to talk about. Balance isn’t what it used to be. Vision or hearing might fade a bit. Medications can make you dizzy. And here’s the tough stat: falls are the top cause of injury for folks 65 and older. In recent years, over 14 million older adults that’s one in four reported falling at least once. Worse, fall-related deaths have climbed sharply, with over 41,000 in 2023 alone.
These aren’t just numbers. A bad fall can mean hospital stays, surgery, or losing the ability to live independently. But here’s the good news: many of these risks drop when someone reliable is around. Constant supervision, help with moving around, and quick responses to little issues make a huge difference.
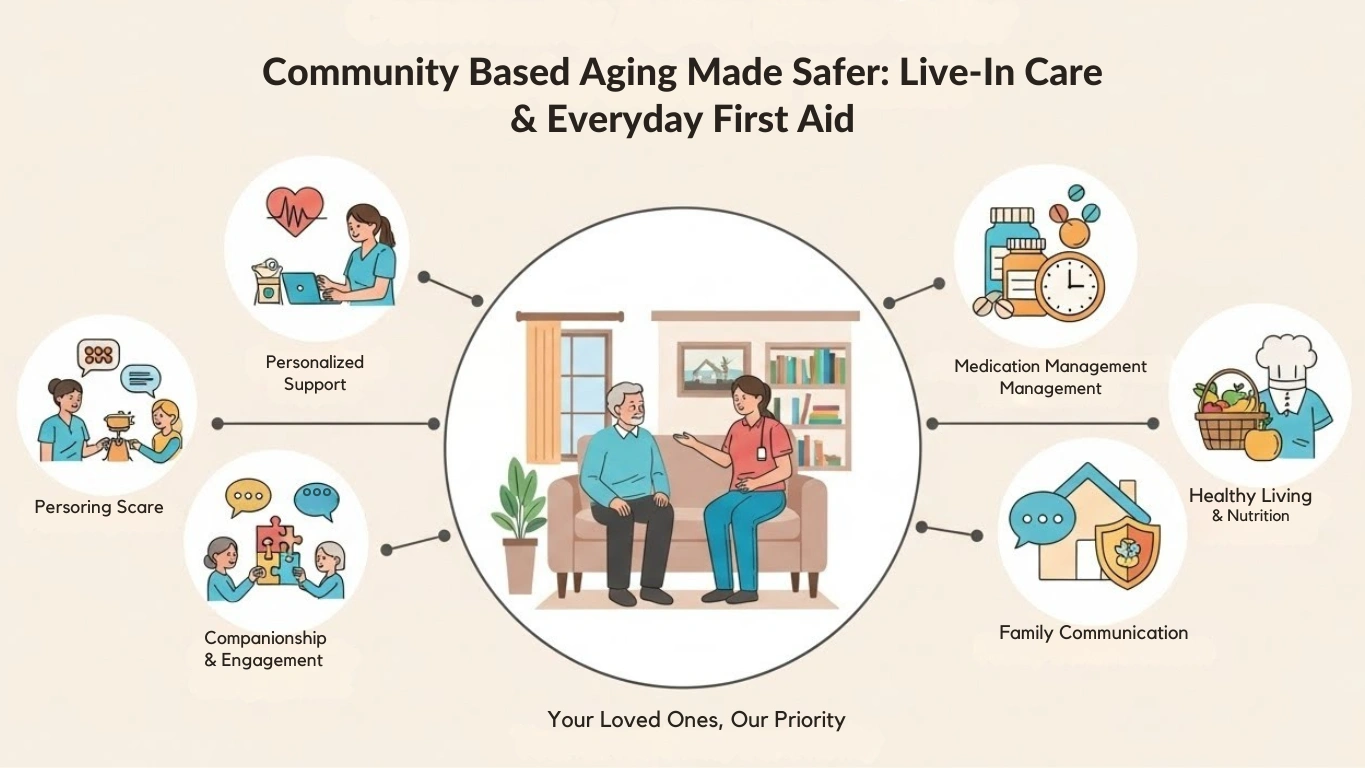
How Live-In Care Changes Everything

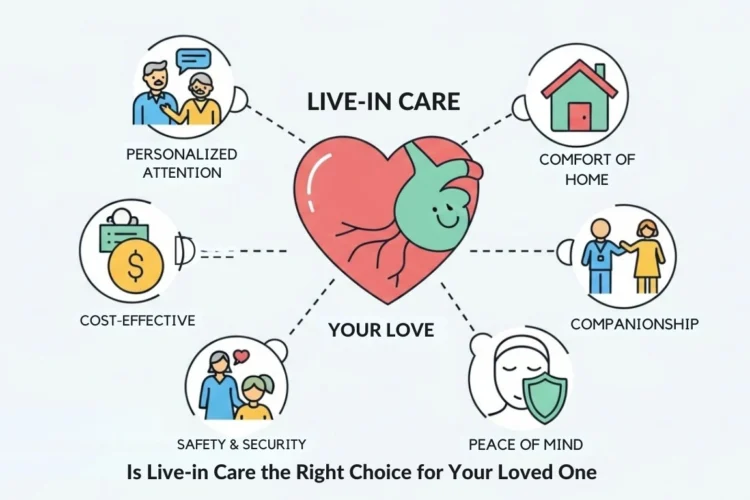
Live-in care means a professional caregiver lives in the home care, ready to help around the clock. They’re there for meals, meds, baths, and just keeping company. Unlike hourly visits, they don’t clock out and leave you alone at night – when a lot of accidents happen.
Families love this because it lets their loved one stay in the community they know. No stressful moves. No losing touch with friends next door. The caregiver can even drive to local events or help visit neighbors. Research shows staying connected like this fights loneliness, which hits emotional health hard as we age.
The Real Benefits of Live-In Care
Let’s talk about what you actually get. First, safety skyrockets. A caregiver spots risks like loose rugs or missed meds before they turn into problems. They help with walking, getting in and out of bed, or the shower – all spots where falls happen most.
Then there’s the personal side. One-on-one attention builds real trust. Your loved one gets care tailored just for them, not a one-size-fits-all schedule. They eat better, stay more active, and often feel happier. Families breathe easier knowing someone qualified is always there.
Compared to other options, live-in care often costs less than full-time facility care while giving more freedom. And it keeps that vital community link walks in the park you’ve known forever, coffee with the same old friends.
Everyday First Aid Skills That Save the Day
Even with great care, little emergencies pop up. Knowing basic first aid gives you confidence and can prevent small issues from becoming big ones. You don’t need to be a nurse just learn a few key things.
Start with staying calm. Check if the person is responsive and breathing. If something serious happens, call 911 first. Then give care until help arrives.
Handling Common Emergencies at Home
Falls top the list. If your loved one falls, don’t rush to move them if you suspect a head or back injury. Keep them still, cover them with a blanket for warmth, and wait for pros. For minor falls, help them up slowly if they’re okay, then watch for swelling or confusion.
Choking is another scary one, especially at meals. Learn the Heimlich maneuver stand behind them, wrap your arms around their waist, and give quick upward thrusts until the blockage clears.
For cuts or bleeding, press clean cloth firmly on the wound. Raise the area if you can. Most stop with pressure, but deep ones need medical help.
Heat exhaustion or strokes hit in hot weather. Signs include confusion, slurred speech, or one-sided weakness. Cool them down, but get emergency help fast for suspected strokes – time matters hugely.
Burns from cooking happen more than you’d think. Run cool water over minor ones for 10 minutes, then cover loosely. Don’t pop blisters or use ice directly.
Build a Senior-Friendly First Aid Kit
Keep a kit where everyone can reach it. Include bandages in different sizes, gauze pads, adhesive tape, scissors, tweezers, pain relievers like ibuprofen, antiseptic wipes, and gloves. Add personal items like extra meds, a blood pressure cuff, or glucose tester if needed.
Check it twice a year. Toss expired stuff and restock. A simple kit handles most everyday bumps until a doctor steps in.
Adding Smart Technology for Extra Peace of Mind
Here’s something newer that’s making waves: smart home tech. Automatic fall detection pendants call for help if someone falls and can’t press the button. Motion-sensor lights brighten halls at night, cutting trip risks. Smart pill dispensers beep reminders and alert family if doses are missed.
Video doorbells let you see who’s there without hurrying to the door. These tools work great alongside live-in care, giving an extra safety layer without feeling intrusive.
Comparing Your Care Options
Here’s a straightforward comparison to help you weigh choices:
| Care Option: | Key Advantages: | Potential Drawbacks: |
|---|---|---|
| Live-In Care | 24/7 personalized support at home, keeps community ties, builds strong relationships, often more affordable than facilities | Needs space for caregiver, finding the right match takes time |
| Hourly Home Care | Flexible scheduling, good for lighter needs, cheaper for fewer hours | Gaps in coverage, especially nights, multiple caregivers can feel inconsistent |
| Assisted Living Facility | Built-in social activities, on-site medical staff, meals provided | Loss of home and neighborhood, higher costs, less privacy |
FAQs
What exactly does a live-in caregiver do every day?
They help with personal care, meals, light housekeeping, meds, and companionship. They adapt to what your loved one needs most.
Is live-in care more expensive than other options?
It varies by location and needs, but for round-the-clock care, it’s usually cheaper than assisted living while offering more one-on-one attention.
Do I need training to handle first aid at home?
Basic classes from the Red Cross or local groups are quick and worthwhile. They teach confidence without overwhelming you.
Can my loved one still see their old doctor and friends with live-in care?
Absolutely that’s a big plus. The caregiver can drive to appointments or help host visitors.
What if we only need help part-time at first?
Many agencies start with fewer hours and scale up as needs change. It’s flexible.
Aging in your community doesn’t have to mean risking safety. With live-in care and some basic first aid know-how, you create a setup that’s secure, comfortable, and full of the connections that matter most. It’s about living well, not just hanging on. If you’re navigating this for someone you love, take it one step at a time you’ve got this.



A WordPress Commenter
June 18, 2025Hi, this is a comment.
To get started with moderating, editing, and deleting comments, please visit the Comments screen in the dashboard.
Commenter avatars come from Gravatar.